- Fares Laroui
- March 4, 2021
What is interprofessional collaboration in healthcare? And why is it important?
Getting individuals and teams to collaborate effectively on an ongoing basis is among the top priorities for many organizations regardless of their size and industry.
The reason is simple. If done right, collaboration can prove to be the difference between success and failure. And in the case of the healthcare industry, collaboration is vital to facilitate the exchange of critical knowledge, provide better patient care and potentially save lives.
However, achieving great levels of collaboration and team cohesion between healthcare practitioners is by no means an easy feat. It requires a combination of policies, best practices and tools that can help teams work better together.

Content
In this blog post, we will cover three main questions:
(1) What is the concept of interprofessional collaboration in healthcare?
(2) Why is it important?
(3) How can digital workplace solutions support interprofessional collaboration?
1. What is interprofessional collaboration in healthcare?
This type of collaboration can bring a host of benefits to the involved parties. Collaborating with people from different areas of expertise can help to eliminate bias, widen perspectives and drive innovation. This eventually leads to effective decision making, better offerings and improved customer service.
For example, think of a typical hospital set-up. Any given patient would be taken care of by multiple health practitioners, such as doctors, nurses, pharmacists, and so on. In order for the involved parties to reach their common objective (which is to treat the patient) and eliminate medical errors associated with poor communication, they need to communicate, collaborate and share knowledge in real time.
2. Why is interprofessional collaboration important?
Improve the overall patient journey
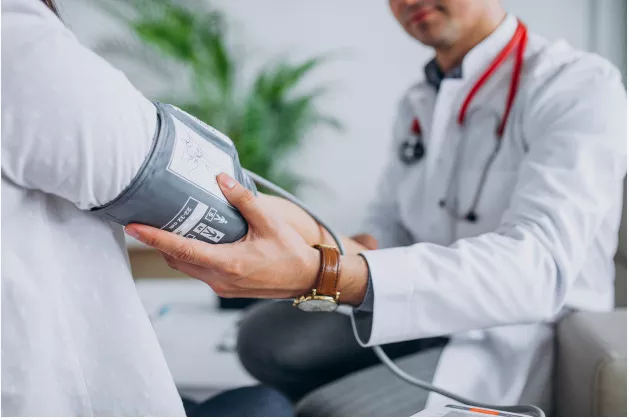
A patient journey represents the various events and activities that a patient has to navigate within a typical healthcare system. It starts with an appointment, scheduling all the way to tests, diagnosis, eventual treatment and follow-up.
Each event within the patient journey requires continuous collaboration between the involved parties (healthcare staff, patients, families and the community). This is when interprofessional collaboration happens.
For example, let’s walk through a typical patient experience. Usually, when patients visit a hospital, they will be taken care of by the ER or they may have already booked an appointment via a phone call to see a doctor. In both cases and depending on the condition, they can be transferred to another department for tests (blood tests, scans, etc.) to further understand their condition.
Although patients have their unique records that will eventually follow them within their stay, their condition and symptoms may change in a matter of hours, which makes it hard to synchronize efforts between rotating nurses, doctors, radiologists and others, each of whom have their unique experience and expertise that may contribute to identifying the right treatment at the right time.
The only challenge, though, is that these different teams don’t necessarily have the same working schedule and solely rely on the patients’ files, which can become obsolete or outdated if the condition at hand evolves quickly.
The solution for many hospitals is to provide and create the right environment that will foster collaboration and encourage healthcare professionals to join their efforts to streamline the patient journey and improve decision making and the quality of care. To achieve this, many entities of the healthcare ecosystem started to restructure their teams, taking into consideration collaboration best practices and frameworks (such as SABR among others) and deploying specialized tools with the potential to support such initiatives. f you’re interested in the best way to strategically retain patients, you should absolutely be making improvements to the patient journey. After all, a patient who’s able to get the care they need in a reasonable time frame won’t be leaving your practice anytime soon.
Facilitate access to critical information
In order to provide the highest quality of care and prevent medical errors, healthcare professionals working jointly on a specific case need easy and timely access to critical information.
As mentioned earlier, a failure to gather valuable insights from other teams may slow the treatment process or lead to inaccurate diagnosis, which poses a threat to patients’ health and safety.
For example, the absence of a centralized knowledge base or adequate communication channels may lead important documents such as test results to be lost in endless email threads or paperwork, which is not ideal, especially in critical cases.
With the right collaborative practices and tools in place to support interprofessional collaboration, different teams can speed up the onboarding and diagnosis phases and quickly move to intervention and treatment.
Encourage the exchange of expertise

Getting individuals with different backgrounds and experiences to work together isn’t a guarantee of success. Multiple issues can result from this collaboration, especially if there haven’t been any frameworks or guidelines in place to help organize this process.
Each individual may have his/her own beliefs, points of view and vision on how to deal with certain situations. Add to that biases associated with each profession and a lack of knowledge of peers’ work or added value, and this collaboration may carry more harm than good for everyone involved.
The very essence of a fruitful interprofessional collaboration is the ability of healthcare professionals to understand their own roles and responsibilities as well as those of their counterparts. This will eventually pave the way to knowledge sharing and the exchange of expertise as each professional has a detailed understanding of what they can bring to the table and how they can help their peers or benefit from their expertise.
In some cases, collaboration may need to extend beyond just healthcare teams. For example, patients with conditions like cerebral palsy may benefit from both medical care and legal support from a cerebral palsy attorney. Taking an interdisciplinary approach and identifying relevant specialty resources can optimize outcomes.
Eliminate communication silos

Communication silos and disconnected teams and departments are arguably among the most recurrent challenges for many industries, especially healthcare.
Traditionally, healthcare professionals had neither the right techniques nor the tools to streamline communication and only referred to patients’ charts and records to keep track of patient status. This often leads to inaccuracies and errors, reduces cost efficiency and affects the overall quality of care.
Ideally, teams involved in a specific case would place the patients’ needs at the heart of their operations and would collaborate and coordinate accordingly. Yet, this is easier said than done. As we mentioned earlier, there are a host of barriers (be it organizational, financial, technological and, of course, human) that hinder collaboration.
When provided with communication tools designed for the healthcare industry and, of course, the right frameworks, healthcare teams would be able to operate in harmony, synchronize their interventions and stay up to date with various information that not only relates to the cases at hand but also to the entire hospital network (news, events, latest research studies, training material, etc.).
Prevent medical errors
As the third leading cause of death behind heart disease and cancer, according to a Johns Hopkins research study, medical errors are a major concern for healthcare institutions.
Medical errors are due to multiple causes, ranging from poor communication and limited access to timely knowledge, all the way to lapses of concentration, stress and burnout, among others.
Regardless of the cause, be it intrinsic or extrinsic, interprofessional collaboration plays an important role in preventing medical errors, and guarantees the safety of patients.
For example, if the error is caused by the absence of a clear communication model that, in turn, resulted in a mis- or late diagnosis, this can be rectified by first setting clear goals and expectations and, secondly, supporting these by ensuring adequate frameworks, tools and the right individuals are in place.
Engage medical staff and avoid burnout
A number of studies conducted to measure the engagement of healthcare professionals revealed some worrying statistics. For instance, one Harvard report found that half of all doctors surveyed reported symptoms often correlated with burnout at work, such as depression, exhaustion and job dissatisfaction. Another study conducted on nursing engagement found that 14.4% of nurses feel disengaged, with a further 41% feeling burnt out.
Burnout in any profession – and especially healthcare – can have severe consequences on the levels of care provided, and can lead to medical errors.
Long hour shifts and being constantly in the frontlines (especially during the times of Covid-19), along with high demands and expectations – both in terms of the job itself as well as the emotional investment in talking with and comforting patients – can lead healthcare personnel to feel overwhelmed and burnt out.
To effectively face this challenge, many healthcare organizations are investing heavily in both process and software that will help them first measure the levels of engagement and well-being and then act accordingly.
Having the floor that will promote and favour interprofessional collaboration is key to helping employees feel empowered and engaged at work. Being part of a team and having clear expectations and clear processes in place, along with a transparent culture, is proven to limit burnout, engage workers, improve job satisfaction and reduce turnover rates.
3. How does the digital workplace support interprofessional collaboration?

As a highly regulated industry with different teams collaborating daily on critical information such as patient records, documentation, invoices, test results, and so on, healthcare institutions require a combination of tools to better manage and organize their operations (for example: FHIR server).
From communication and collaborative solutions, all the way to knowledge, project management and portals, the possibilities are endless for healthcare IT buyers.
However, decision makers should be wary about collaborative tool overload – a phenomenon that has seen many organizations spend heavily on a collection of software solutions for little to no return since employees are trapped in a never-ending loop of software applications and platforms.
They eliminate communication silos through social and content management features such as news and microblogs;
They create a rich knowledge base, where staff can easily and quickly locate and find what they are looking for, thereby speeding up intervention and treatment times;
They enable people to collaborate within spaces that can be dedicated to either teams, departments or entire clinics, where staff can share updates in real time on specific cases and share any questions or training materials.
Provide patients with a patients portal that will allow them to get in touch with their medical staff and avoid any confusions regarding appointments, scheduling and any other procedures.
Measure engagement with analytics features and build tailored engagement, recognition and gamification programs
Provide frontline and deskless employees with a mobile solution containing everything they need to communicate and collaborate instantly.
FAQs
You will find here Frequently Asked Questions about collaboration with all the answers in one place.
What is collaboration?
Collaboration is “the situation of two or more people working together to create or achieve the same thing”.
What are the different types of collaboration in business?
Here are some definitions of digital workplace:
- Team collaboration
- Cross-departmental and interdisciplinary collaboration
- Community collaboration
- Strategic partnerships and alliances
- Supply chain collaboration
How to choose the best type of collaboration?
In order to effectively find the right type of collaboration for your business, you have to follow a strategic approach and answer three common yet critical questions: Where are we? Where do we want to be? And how to get there?
Why collaboration is important?
At the internal level, businesses try to encourage and seek to incorporate different forms of collaboration in the workplace to lay the foundations for teams to be able to work together with an aim to achieve higher levels of success.
Externally, businesses look to engage in collaborative actions to benefit from others’ expertise, to gather the opinions of their customer base and to get customers and other stakeholders more involved in the development of products and services.
What are the benefits of collaboration in the workplace?
Here are some of the benefits of collaboration in the workplace:
- Foster innovation and creativity
- Better problem solving
- Effectively handle times of crises
- Engage and align teams
- Increase motivation
- Attract talents
- Tags: Digital workplace, Collaboration
Related posts
- All
- eXo
- Digital workplace
- Employee engagement
- Open source
- Future of work
- Internal communication
- Collaboration
- News
- intranet
- workplace
- Knowledge management
- Employee experience
- Employee productivity
- onboarding
- Employee recognition
- Change management
- Cartoon
- Digital transformation
- Infographic
- Remote work
- Industry trends
- Product News
- Thought leadership
- Tips & Tricks
- Tutorial
- Uncategorized
Leave a Reply
( Your e-mail address will not be published)